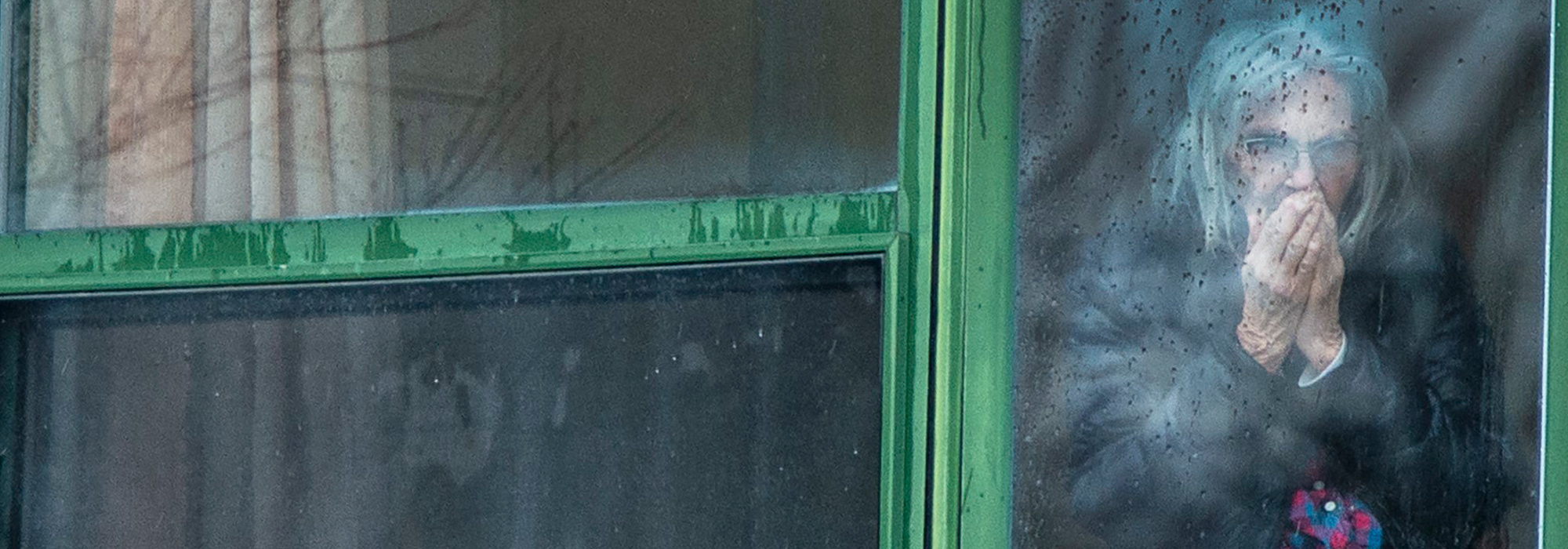
It’s bad news for civil rights when a government decides to sentence an entire population to house arrest, but for long-term care residents this pandemic policy is not new. For them, long-term has always meant lockdown. Life is a desert of boredom and loneliness for many institutionalized Canadian seniors. Those who express frustration and restlessness are often subdued with medication. A shocking 60 percent are drugged by antidepressants, according to the Canadian Institute for Health Information, a rate about twice as high as among seniors in the community. Yet depression is a normal response to powerlessness, solitude and empty days with nothing to look forward to.
Canadians were appalled to learn in spring 2020 about the extreme neglect of bed-bound and wheelchair-bound patients in some long-term care homes, but this tragedy is not the only failing of the industry. In many care homes, confinement to individual rooms is regular practice, even for ambulatory patients. At the end of purposeful and contributing lives, they’ve become prisoners in the anteroom of death. They deserve better, epidemic or no epidemic. To many, getting the virus would not be the worst outcome; many express a wish to die.
Not all elders in long-term care are bedridden or suffering advanced Alzheimer’s disease. Diseases of aging have stages, and many patients eat and walk independently. The meal put on the table in front of them three times a day is sometimes the only event that happens, the walk up and down the same stretch of hallway behind a locked door the only exercise, and the irrelevant chatter of TV the only companionship (many a chat show is more mindless than the patient plunked down in front of it). Before COVID, these people were already experiencing an epidemic — of toxic boredom. Maybe the light shone on the abuses in some care homes, especially in reports from the Armed Forces in May, will illuminate the other shortfalls of the system.
When my mother lived in a care home for dementia patients, I saw residents fighting caregivers — the residents alternately screaming and clamping their mouths shut — who were literally forcing pills down their throats. When I expressed alarm to administrators, they told me they couldn’t discuss this because of patients’ “privacy rights.” It seems patients have rights to privacy but not to control over what goes into their bodies. My family struggled to limit the opioids given to my mother, who told us she hated feeling sleepy all day: “I never wake up.” Residents without vigilant relatives have no one to monitor overmedicating and other issues of their living conditions. The “vigilant relatives” are of course looked upon by medical professionals as ignorant meddlers — but who else have care home inmates got to advocate for them?
Although the Canadian Constitution defends equality for all, the semi-senile and frail institution-bound elderly seem excluded. Public health officials speak as if infection control is the beginning and end of their responsibility. It isn’t. The gerontology profession needs to support care home residents’ civil rights.
Some organizations do concern themselves with these residents’ rights, such as the National Initiative for the Care of the Elderly. Based at the University of Toronto, NICE asserts that “there is a gap between what evidence has shown to be best practice in the care of the elderly, and how practice is truly carried out.”
The Canadian Centre for Elder Law also aims for reform and states that “some people assume that if you have dementia you cannot understand information or make choices,” an assumption that “happens within health care institutions.” As a family visitor and a memoirs coach in care homes, I have witnessed plenty of understanding among residents, and also their feeling that their lives have lost meaning.
Many Canadians are experiencing depression and loneliness during the COVID-19 lockdown. They’ve turned to gardening, walks with physical distancing, videos, talking books, mindfulness practices, phone calls with friends. Why haven’t care home inmates got these, since every day is lockdown day for them? If COVID-19 does nothing else, maybe the enforced isolation it has brought to the public at large will make people think about isolation among the institutionalized elderly. If studies occasioned by COVID-19 on the mental health effects of loneliness and boredom lead to understanding the plight of long-term care residents, some good will have come out of the pandemic.

Under Canadian common law, doctors only recommend treatments; consent lies with patients. “Across Canada, treatment without consent is a form of battery,” states a May 2020 article by the British Columbia Law Institute, a research and information umbrella organization under which the Canadian Centre for Elder Law works. Its statement about battery is relevant to both drug prescribing and isolation procedure; the article notes that “health care consent rights…may indicate a need to relax rules around physical distancing to support decisional autonomy” of patients.
Isolation rules are not new; care homes regularly enforce them during norovirus, influenza and other outbreaks, but the pandemic has made them universal. How might they be relaxed? It wouldn’t be difficult: new care home staff could be hired exclusively as socializers, entertainers and conversationalists. Conversation is vital for mental health, as important as food preparation and bath giving.
And why not hire folks who have lost other jobs, to take residents one by one on a daily exercise circuit around the garden? The benefits of time spent in natural settings are well documented.
It should also be possible for relatives, duly masked and hand-washed, to visit residents in private rooms. Musical groups wanting performance opportunities could set up in parking lots so inmates could watch a show.
There has been discussion about caregivers’ working conditions and the possibility of raising their wages. This won’t necessarily help residents, however. Reform has to be shaped around them, and it starts with observers being allowed inside care facilities. Family members and the public need to exercise oversight. After all, we’ll only be overseeing what will one day be the end-of-life living conditions for many of us.
This article is part of the Facing up to Canada’s long-term care policy crisis special feature.
For related content, check out the IRPP’s Faces of Aging research program.