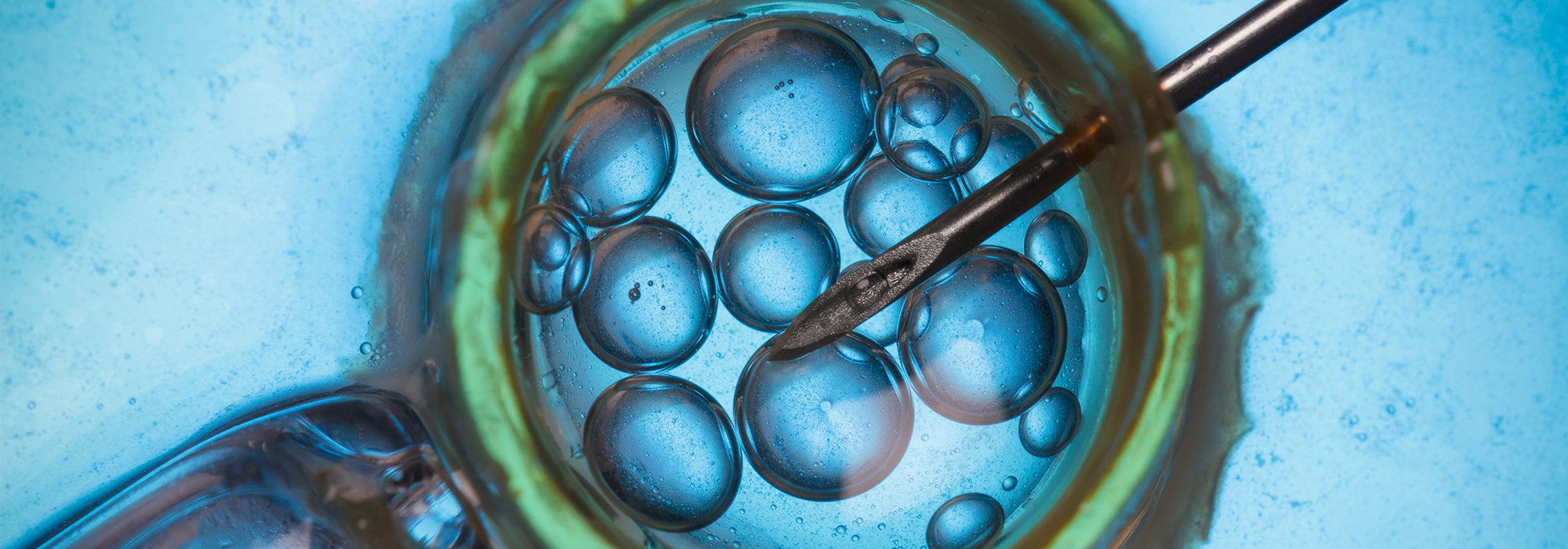
In-vitro fertilization (IVF) has come a long way since the birth of the first test-tube baby in England in 1978. IVF is a procedure in which eggs are removed from a woman’s ovary and fertilized with sperm in a laboratory dish. The embryos are transferred to the woman’s uterus. They can also be donated to another woman or couple, or used for research purposes. Once an experimental procedure, IVF is now considered the mainstay of reproductive medicine. In 2017, over 36 IVF clinics initiated over 33,000 IVF cycles in Canada. It has been estimated that approximately 1 to 2 percent of live births in Canada result from IVF and related treatments.
Despite the routinization of IVF, the procedure remains expensive. An IVF cycle can cost $10,000 to $20,000, depending on the amount of medication and use of other procedures, such as prenatal diagnostic testing, embryo freezing and storage. Given rising health care costs, who should pay for IVF treatments?
In many countries, such as Australia, Sweden and the UK, publicly funded IVF treatments is available to infertile couples. In Canada, however, only Ontario provides limited coverage, offering one IVF cycle under its health insurance plan. Quebec introduced a publicly funded IVF program in 2010 only to terminate it five years later due to an unexpected jump in the program’s costs. Quebec, New Brunswick and Manitoba are now the only provinces that offer tax credits to help patients offset some of their fertility treatment costs. In the rest of the country, patients must pay for IVF on their own.
Part of the reason why IVF is not publicly funded is that although infertility is understood to be a medical condition, IVF is not considered a medical necessity. The Canada Health Act mandates provinces to provide coverage only for treatments and services deemed to be “medically necessary.” The term, however, is not defined in the Act. Provinces are left with considerable leeway in interpreting which services they must cover. Although provinces pay for treatments such as surgeries to address the underlying causes of infertility, only Ontario regards IVF as medically necessary.
The consequences of not publicly funding IVF are several. First, by not insuring IVF, governments have unwittingly turned it into a private commodity rather than a medical service. In its 1993 report, Canada’s Royal Commission on New Reproductive Technologies recommended against privatizing IVF treatments, due to concerns over the commercialization of reproduction. But despite the commission’s warning, money determines who can get reproductive treatments today and who does not. Access is restricted to wealthier, often white couples, disadvantaging poorer women and couples who cannot afford to pay the fees charged by private clinics.
Second, there is minimal government oversight of IVF clinics, except in Quebec. At the federal level, the 2006 Assisted Human Reproduction Act (AHRA) did contain provisions for licensing and monitoring IVF clinics, but they were struck down by the Supreme Court in 2010 because they were deemed to encroach on provincial jurisdiction.
Public funding of IVF would offer another way to improve safety and quality of IVF services and could lower health care costs in the long term because governments could impose restrictions. Sweden, for example, which publicly funds IVF, discourages multiple births since they present greater health risks and higher health care costs; it legally mandates single embryo transfers for younger patients. Driven by similar concerns, Ontario’s program allows only single embryo transfers. When patients are not influenced by financial considerations, they no longer feel the pressure to opt for multiple embryo transfers in the hopes of achieving a successful pregnancy.
Third, eligibility criteria for IVF can vary from clinic to clinic. Although guidelines from medical groups, such as the Canadian Fertility and Andrology Society, do exist, individual clinics often set their own limits for age and weight. In Ontario, for example, some clinics use body mass index to determine eligibility while others have no cut-offs at all. Public funding would help establish more consistent, uniform and transparent criteria across clinics located in the same jurisdiction.
Finally, although the AHRA states that persons cannot be denied access to IVF on the basis of sexual orientation or marital status, barriers continue to exist for disadvantaged or marginalized groups. For example, services and information materials used by IVF clinics are often not inclusive of LGBTQB+ patients. Providing public coverage for IVF could help ensure that clinics provide services that do not reinforce health inequities based on race, ethnicity, gender identity and sexual orientation.
Public funding of IVF can level the baby-making playing field by making the treatment accessible to low-income individuals and couples. It can also provide for greater oversight and protections for patients and for more consistent eligibility requirements. Still, public coverage of IVF alone would not fill all the gaps that currently exist in assisted human reproduction policy. It would not, for example, resolve issues related to elective egg freezing, the status of frozen embryos, reimbursement for egg or sperm donors, or surrogacy arrangements. To fill the void, both levels of government need to step up their efforts and work together to implement a regulatory framework for assisted human reproduction.
This article is part of the Addressing the Gaps in Canada’s Assisted Reproduction Policy special feature.
Photo: Shutterstock by nevodka
Do you have something to say about the article you just read? Be part of the Policy Options discussion, and send in your own submission. Here is a link on how to do it. | Souhaitez-vous réagir à cet article ? Joignez-vous aux débats d’Options politiques et soumettez-nous votre texte en suivant ces directives.