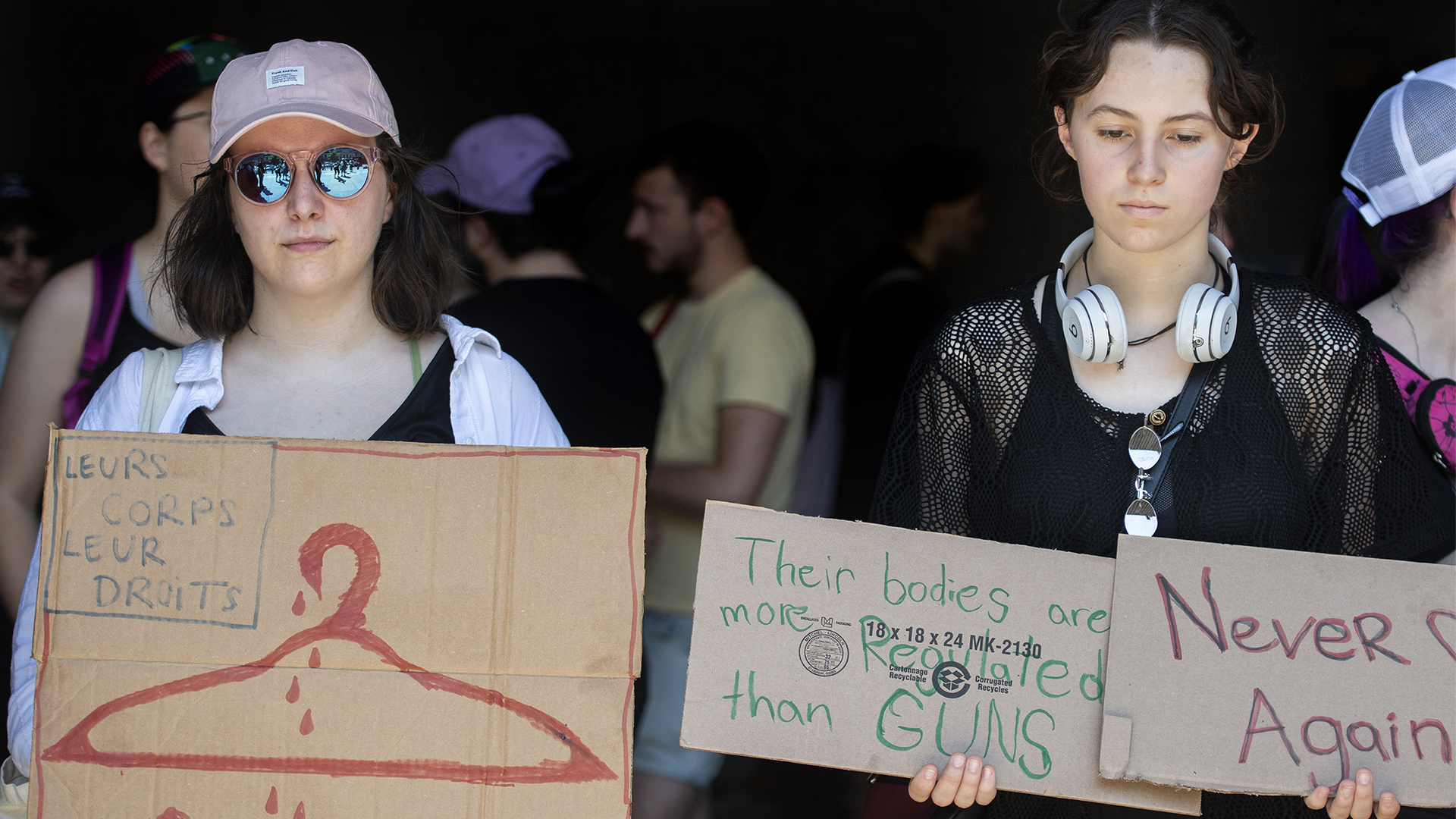
The U.S. Supreme Court’s decision to overturn Roe v. Wade – an attack on the rights of women and 2SLGBTQQIA+ people who can get pregnant in America – has sent shockwaves of fear and grief across the globe. Nearly half of all states have laws that can restrict access to legal abortions with 13 having pre-existing “trigger laws” to outlaw abortion, which kicked in when Roe v. Wade was overturned. Now women and the 2SLGBTQQIA+ community in Canada are left wondering whether we are vulnerable to the same regressive, anti-choice influences.
We can be comforted by the fact that abortion is decriminalized in Canada, with no legal requirements such as parental consent or waiting periods that can prevent access. Karina Gould, minister of families, children and social development, has said Americans could travel to Canada to receive an abortion, which may lead to an influx of U.S. patients to Canada.
However, Canada is not the safe haven for abortion it may seem. The organization of Canada’s health-care system, the dearth of abortion providers across the country and the prevalence of anti-choice organizations combine to make access difficult if not impossible in some cases. The onus is on patients to find the care they need. With abortion being one of the most common medical procedures in Canada, this is entirely unacceptable.
Put abortion pills into people’s hands
Those who live in rural areas, especially those living on reserves, have almost no access. Abortion clinics in Canada are concentrated along the U.S. border and only one-in-six hospitals provides abortion care.
As a result, people in rural communities do not have access to nearby care and are forced to travel to receive what they need. This is especially true for provinces such as Alberta, Manitoba, Saskatchewan and Ontario, where 35 to 40 per cent of individuals live in remote communities or in rural areas.
A Canadian study from 2013 found that 18.1 per cent of women travelled more than 100 kilometres to access abortion, with Indigenous women being three times more likely than white women to have travelled this distance. This puts those without the financial and logistical means to travel at a disadvantage and further exacerbates issues of inequitable access.
Provincial guidelines also contribute to this inequity. Nearly 90 per cent of all abortions in Canada occur before 12 weeks. Yet some individuals may require abortion care beyond this gestational period and whether they can access it depends on their home province. P.E.I., for example, is the most restrictive, with abortion becoming inaccessible after 12 weeks.
Even though abortion rates decline after this period, it is still critical that the option is accessible. A decision to terminate later may be made for personal reasons, medical concerns, or factors outside of the person’s control – including transportation difficulties, limited access to accurate pregnancy tests, or desperate domestic circumstances. Currently, abortion care at 20 weeks is available only in B.C., Alberta, Ontario and Quebec. After 24 weeks, individuals are forced to leave the country to seek safe care – a luxury reserved for a privileged few.
Insurance coverage, or the lack thereof, also affects access. Nunavut, for example, does not offer coverage for medical abortions except for select cases, such as those prescribed in hospitals. Similarly, in New Brunswick and Nova Scotia, those accessing surgical services through freestanding abortion clinics must pay out-of-pocket. Abortion is one of only 16 medical procedures exempt from “portability” under the Canada Health Act (CHA).
Portability allows services under provincial health plans to be covered even outside the individual’s home province. With abortion, however, those forced to travel outside their home province to access care are stuck with a bill for a service that should be covered under medicare.
Compounding the issue of inequitable abortion access are unregulated crisis pregnancy centres (CPCs). CPCs are anti-choice wolves in sheep’s clothing. They are advertised as a resource for individuals with unplanned pregnancies to receive support and counselling. However, they deceive clients with misinformation about abortion or other options that may delay or interfere with their ability to access the care they need.
CPCs far outnumber abortion care providers in Canada. In Ontario alone, there are 77 active CPCs but only 38 abortion providers. Overall, in Canada, there are 165 CPCs compared to 147 abortion providers. This means an unwitting pregnant person seeking an abortion is more likely to come across a CPC than an abortion provider for information. Considering geographical and gestational barriers to care, time is of the essence for any pregnant person to exercise the right to choose.
It is disturbing that in a country with legal and (mostly) publicly funded abortion, we still face massive hurdles to obtaining care. So how do we move forward to improve access in Canada? Let’s start with funding. Why are we, members of a pro-choice non-profit focused on evidence-based education, competing for funding with anti-choice groups such as the CPCs? We heard promises that were included in the Liberal platform in 2021 to prevent anti-choice groups and CPCs from being assigned charitable status, but we have yet to see these promises kept.
One recommendation is not to limit who can obtain “charitable” status, but instead restrict what types of charities can receive donations and tax exemptions from a values-based perspective. Religious groups focused on charitable issues could still receive funding, but those imposing religious beliefs on others would not.
We commend the federal government for announcing $3.5 million in funding for Action Canada and the National Abortion Federation Canada since Roe v. Wade was overturned. Let’s continue to build on these progressive steps. Health Minister Jean-Yves Duclos must consider funding smaller, community-led organizations to help improve regional abortion access and education.
But funding is only half the battle. We also urge federal and provincial governments to treat abortion like the medically necessary procedure it is by firmly situating abortion within the CHA. All provinces and territories have deemed abortion a medically necessary procedure – meaning it currently falls under the CHAs broad definition of “insured health services.”
For provinces and territories to receive full funding through the Canada Health Transfer, they must meet CHA criteria and conditions for all insured health services, such as full funding and accessibility. However, as we and countless others have pointed out, abortion is not accessible. Our governments are failing us.
Some provinces do not fund abortions provided outside of hospitals, and others force patients to pay for services at private clinics or incur other costs to obtain an abortion. These are violations of the CHA, under which the federal government has an obligation to intervene.
We must call on provincial and federal representatives to ensure compliance with the CHA and to address significant barriers to receiving an abortion in Canada. Funding must improve to cover all of the costs associated with accessing abortion services. As well, the scope of practice for health-care professionals such as nurses and midwives could be potentially expanded to provide abortions.
To hold provinces accountable, the federal government must impose more severe funding restrictions on those who do not take actionable steps to improve access. The decision to penalize New Brunswick by withholding slightly more than $140,000 in health-care transfers is not enough.
Canada likes to think of itself as a beacon for those escaping the implications of Roe v. Wade in the United States. But there are still concerns that all women and members of the 2SLGBTQQIA+ community are not being provided equal access, particularly if they live in rural or remote areas of Canada. It’s time our governments acknowledge that without equitable access, abortion is a right reserved only for the privileged few.
The authors would like to also acknowledge the contributions of missINFORMED’s advisory chair, Nipa Chauhan, who supported this piece as an editor. Chauhan holds a master of health sciences in bioethics from the University of Toronto and works at Mount Sinai Hospital as a bioethics associate.