
The field of childhood chronic conditions is undergoing a sea change. Several recent concepts challenge clinicians and policy-makers to reconsider traditional biomedical thinking (“diagnose/treat/try to fix”) and to create new approaches. What are these concepts and why are they important to children with disabilities and to all Canadians?
Three international developments require attention and application by Canadian policy-makers. The 1989 United Nations Convention on the Rights of the Child explicitly underscores the dignity and equal rights of all children at all times, regardless of background. The 2006 UN Convention on the Rights of Persons with Disabilities reinforces the rights of persons with disabilities outlined in previous declarations, and clarifies those rights. The World Health Organization’s 2001 International Classification of Functioning, Disability and Health (ICF) provides a biopsychosocial framework for health applicable to everyone (figure 1).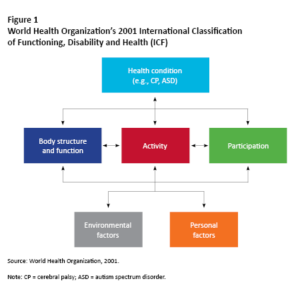
There are four important corollaries of these ideas. First, people now recognize family as the “unit of interest” in chronic childhood conditions; hence, the value of family-centred services (FCS). Research supports the positive impacts of better FCS on parental well-being, stress reduction and satisfaction with services. FCS is an essential underpinning of all services at every level, from the behaviour of front-line clinicians to programs and policies. Family well-being must be a primary goal of all services and programs.
Second, the field is moving beyond diagnosis as the sole driver of services. We now conceptualize childhood disabilities in terms of development and functioning, and not just as biomedical problems to be diagnosed and “treated.” We are adopting a noncategorical approach that recognizes the myriad commonalities across conditions, and the huge variation in manifestations and functioning within any diagnostic category. This capability approach leads to identifying the unfairness of policies and programs that privilege certain diagnostic or lobby groups over others (and to asking whether such privileging is ethical).
Third, there is a profound shift in philosophy of treatment from fixing to functioning and participation. Canadians with disabilities and their families want support to live the best lives they can. For services to be helpful, we need a new definition of treatment success, one that focuses on child- and family-identified goals and the importance of meaningful engagement in everyday life. When we offer services based on ICF concepts, we recognize opportunities to intervene anywhere. For example, we might start by encouraging participation rather than by treating body structure and function. And then we need to look for impacts elsewhere in the interconnected parts of the ICF.
Fourth, we are recognizing the importance of a life-course perspective on childhood disability. Children with child-onset impairments become adults with those impairments, but services and policies have traditionally viewed these conditions only through the lens of children’s medical, educational and therapeutic services. Adult services are woefully lacking: the metaphor used internationally by families of these young people is that “they fall off the cliff at age 18.”
Modern thinking: The “F-words” in childhood disability
The “F-words in childhood disability” (figure 2) won’t fill up anyone’s swear jar! The key ideas — fitness, function, friends, family, fun and future — were created by Peter Rosenbaum and Jan Willem Gorter and grafted onto the ICF framework; they are now known and used across the world.
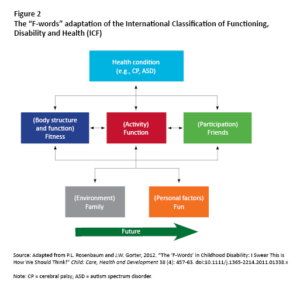
The ICF, together with the plain-language interpretation with F-words, promotes dignity, autonomy and respect for children with disabilities and their families. The F-words support the UN conventions by underscoring the importance of people’s right to equal opportunities, including the right to full engagement in their community and society. Numerous service providers and organizations are using the F-words to set collaborative goals with families, and many are changing the philosophy and structure of their services to support the implementation of these ideas (see CanChild’s “F-words” Knowledge Hub).
At the CanChild Centre for Childhood Disability Research, we believe that all programs and policies for children and youth with developmental disabilities should be grounded in the ICF as operationalized by the “F-words in childhood disability.” Following this framework leads to a focus beyond the individual child to the child-in-family by emphasizing the centrality of these six key elements when planning programs and services. Recognizing the commonalities across developmental conditions can lead to the equitable funding of all programs and services. Finally, although the ICF presents a point-in-time picture of a child’s situation, service and program providers need to acknowledge that developmental disabilities are lifelong realities and that they need to create and maintain programs that extend throughout adulthood.
A call to action
Application of the ICF/F-words framework advances ways of thinking about health policy development and implementation, in the context of health equity and equality. Without this critical examination, we perpetuate unsupportive ways of living for children with disabilities and their families. We must continue to shift the thinking about childhood disability. As one young adult featured in a video about Ontario youth with disabilities urges: “I really want people to think about the possibilities for people with impairments, and never never never to limit someone who has a disability — because they will prove you wrong every single time!”
This article was written on behalf of the CanChild F-words Advocacy Group, including parents and health services researchers. Members include Sherry Caldwell, Danijela Grahovac, Julia Hanes, Manda Krpan Mesic, Rachel Martens, Kinga Pozniak, Alice Soper, Rachel Teplicky and Donna Thomson.
Photo: Kian Snyder, who lives with Severe Cerebral Palsy, rides on the sidewalk outside the Hospital for Sick Children in Toronto. By Samadhi Mora Severino.
Do you have something to say about the article you just read? Be part of the Policy Options discussion, and send in your own submission. Here is a link on how to do it. | Souhaitez-vous réagir à cet article ? Joignez-vous aux débats d’Options politiques et soumettez-nous votre texte en suivant ces directives.







